Successful Transplant of Pig Heart May be Key to Addressing Organ Shortage
On the morning of January 7th 2022, surgeons at the University of Maryland Medical Center removed a heart from a genetically modified pig. They then proceeded to use it for a 7 hour surgery which saw the pig heart being implanted in a human patient successfully, a monumental achievement for the medical community as it offers a possible solution to the persisting shortage of organ donors. The patient, a 57-year-old handy man by the name of David Bennett Sr., had been suffering from terminal heart disease. At the time of the surgery, Benett had been bedridden for several months in the hospital and showing signs of heart failure, a signal indicating that his condition was severe and only going to worsen over time. Because of this, he was barred from both having a traditional heart transplant and using an artificial heart pump.

Elaborating on this further, Dr. Bartley P. Griffith of UMD school medicine said this in an interview with Good Morning America:“His level of illness probably exceeded our standards for what would be safe for human heart transplantation.”
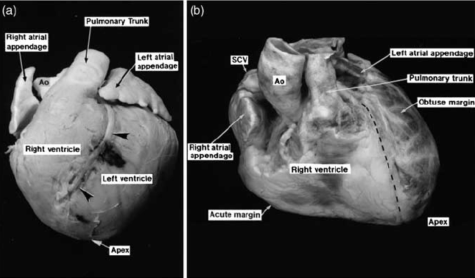
Griffith, a transplant surgeon as well as a professor on the topic, along with a team of researchers had been working for the past five years studying pig hearts and its possible applications in the field. Pig hearts were used because they’re very similar to human hearts anatomically and size wise; they are slightly smaller, but can be easily used as replacement valves.
But, they also carry several risks too. First, The body could see the donated organ as foreign, triggering T-cells and antibodies to damage the organ(organ rejection). The second is the possibility of a danger triggered by the presence of animal cells, tissues, and organs.
To address both, researchers made 10 genetic changes to the heart, including the knocking out certain genes like ones that coded for growth of the heart or the production of carbohydrate epitopes, something that a T-cell would bind to, triggering it to destroy what it sees as foreign matter, which in this case would be the pig heart. 6 human genes were also added.
With his worsening condition and all factors considered, Bennett decided that “It was either die or do this transplant. I want to live.”
On December 31st, 2021 the FDA authorized the emergency use of the pig heart on Bennett, and the surgery was performed little over a week later. As of January 20th, Bennett has remained in stable condition.
Alternatives to human organs for transplant are nothing new. Last year, researchers from NYU langone health attached a genetically modified pig kidney to a woman with no brain activity who was kept alive by a ventilator. They observed the kidney for 54 hours, and reported that it had functioned normally without the body rejecting it.
But the most famous example has to be in 1982 at the University of Utah Medical Center, when Dr. William C. Devries and a surgical team implanted a Jarvik-7 artificial heart made of metal and plastic on Barney Clark, a 61-year-old retired dentist. When the surgery was performed, he was suffering from end stage heart failure. He survived the surgery, and initially there was a veneer of raised hopes and excitement as he was able to speak and breathe on his own. In several interviews soon after his surgery, he had even told the press that he felt comfortable. As the days progressed, he sometimes had trouble breathing and instances of blood pressure dropping, but many maintained that he was still doing more with the artificial heart than without it. But, worsening side effects like seizures and infections, dying 4 months later due to multi-system organ failure. 2 years later, Dr. Devries would perform an artificial heart transplant again on 52-year-old William Schroeder, with a similar sequence of events occurring after. Initially hailed as a success, Schroeder would suffer multiple strokes after the operation, with his deterioration being heavily publicized until his death in 1986.

From the surgery until his death, many questioned the effectiveness in improving a patient’s quality of life, ethics of the heart transplants, and attacked the Jarvik-7 as the medical monster. Some even went as far as to call it “playing god” and, “prolonging the dying process”. In 1990, the FDA withdrew its approval of the Jarvik-7. In 2014, the Jarvik-7 would be re-approved for use as a temporary bridge to heart transplant, now known as the SynCardia temporary total artificial heart.
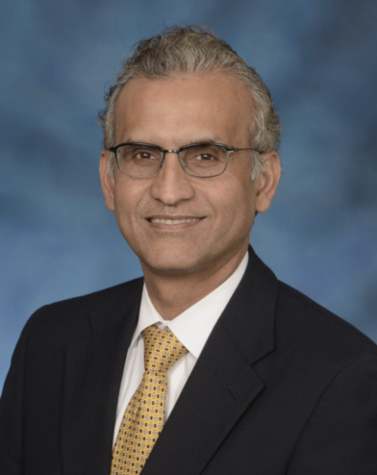
Like Dr. Devries and the Jarvik-7, the recent pig heart transplant has attracted many skeptics and critics. Many have cited concerns about the long term effectiveness of the pig heart, something that cannot be answered and remains to be seen. Others have also cited moral concerns. One of the Doctors involved, Dr. Muhammad Mohuiddin, told the Daily Mail that he’s faced backlash family because he used a pig organ. Him and his family are muslims, and consumption of pork was forbidden. Although Dr. Mohuiddin himself has come to the conclusion that “there’s nothing greater in the eyes of God than saving a human life”, many ethical concerns, similar to the ones Dr. Devries faced, have been raised, and new ones have arisen as the landscape and thought-scape of the world changes.
Overall, the viability of a non-human heart, whether it be artificial (3D printing) or from a different mammal species like a pig heart, still remains to be seen. But, if successful, this transplant and its implications could possibly improve the lives of not just people in need of cardiac transplants, but of the 50,000 people a year that are candidates for all transplants in the midst of an organ shortage crisis that is unable to keep up with demand.






